What Is an Anxiety Disorder?
While anxiety is a normal and healthy reaction to stress, an anxiety disorder is an excessive presentation of fear and anxiety, usually to a disruptive point or where the person’s quality of life is negatively affected on a regular basis.
Anxiety disorders come in many forms. Grouped together, they account for some of the most common mental health disorders.
Today, 3 in 10 adults have some form of anxiety disorder.
Anxiety disorders can present as generalized anxiety disorder (persistent and chronic worry that interferes with daily life), panic disorder (panic attacks), specific phobias, social anxiety disorder (fear of interacting with strangers or fear of being in social situations), and separation anxiety disorder (fear of being left alone or fear of abandonment), among many others.
Anxiety & Substance Abuse
An anxiety disorder does not cause or lead to substance abuse, but the symptoms of the disorder can lead to conditions that make a drug or alcohol addiction more likely to occur.
Many people with some form of anxiety disorder will not start taking drugs or alcohol for recreational purposes. They may start because the substances offer a temporary reprieve for their symptoms. In some cases, a doctor may prescribe medication for the treatment of the anxiety, and then, the person becomes dependent on the medication to feel better.
In any case, taking mind- and mood-altering substances will almost certainly exacerbate the worst symptoms of the anxiety disorder, conversely convincing people that they should take more of the drugs or alcohol to escape the symptoms of anxiety. In many cases, people find themselves trapped in a cycle of anxiety and drug abuse. If this behavior is not stopped in time, the person’s anxiety disorder symptoms and their dependence on drugs or alcohol will deepen considerably.
This phenomenon is well documented. It is “a cycle of self-medication and rebound anxiety,” in the words of Psychology Today. In explaining the relationship, the Anxiety and Depression Association of America writes that anxiety disorders “frequently travel in the company” of substance abuse.
Anxiety Aisorders and Alcohol Abuse
Many people who have social anxiety disorder, for example, drink heavily to make use of alcohol’s nature as a “social lubricant.” Someone with general anxiety disorder may abuse opioids to feel more relaxed and calm.


Understanding the Risk Factors for Substance Abuse
Relationship Factors
In either example, however, the anxiety robs the person of the necessary perspective they need to recognize their limits. A person with social anxiety disorder will find themselves eventually unable to stop drinking for even the most mundane of social interactions. A person with general anxiety disorder will not be able to discontinue their reliance on opioids (whether prescription or illicit) to feel better, eventually becoming fully addicted to not feeling anxious all the time.
One of the many factors that complicates the relationship between substance abuse is that discontinuing the substance abuse (especially after prolonged or intensive use) typically brings its own symptoms, many of which either introduce symptoms of anxiety or exacerbate the symptoms that are already there.
The Behaviour Research & Therapy journal reported that among people who have panic disorder, as many as 40 percent of that population will struggle with alcoholism. Similarly, upward of 20 percent of people who have panic disorder will abuse other substances.
In many of the cases where this occurred, the anxiety symptoms developed before the substance abuse did, but not everyone who develops anxiety disorder will also have co-occurring substance abuse disorder. Those who do will likely have other factors in their family and medical history or their environment that increase the chances of self-medicating with drugs or alcohol than those who don’t. For example, those who don’t attempt to self-medicate might be able to access treatment quicker and easier than those who do.
Treating Both Conditions
When treating co-occurring substance abuse and anxiety disorders, the Social Work in Public Health journal writes that one of the challenges is effectively treating both conditions and not focusing on one ailment at the neglect of the other. In cases like substance abuse and anxiety disorders occurring together, doctors turn to dual diagnosis treatment, a form of intervention and therapy that addresses the complex interactions of both conditions.
Dual diagnosis offers a continuum of care between the substance abuse and the anxiety disorder, so both conditions receive the appropriate degree of treatment, in the appropriate time. This is a reversal of an outdated model of treatment, where a person was expected to achieve stabilization in one condition before they could receive treatment for the other.
Modern research into the intersection between substance abuse and mental health conditions (like anxiety disorders) has shown that this outdated model can lead to relapse. Doctors will now try to treat a co-occurring case of addiction and anxiety disorder simultaneously.
Health care professionals trained in dual diagnosis are specialized in treating addiction and mental health together, so that all elements of the client’s psychological well-being are met. Additionally, people will likely receive both psychotherapy and prescription medication, with one modality complementing the other.
Lastly, key people in the client’s life — their partners/spouses, children, family members, and close friends — will be invited to be involved in therapy. These loved ones can provide a support and accountability network for the client to rely on when they are discharged from treatment.
The Role of Neurotransmitters
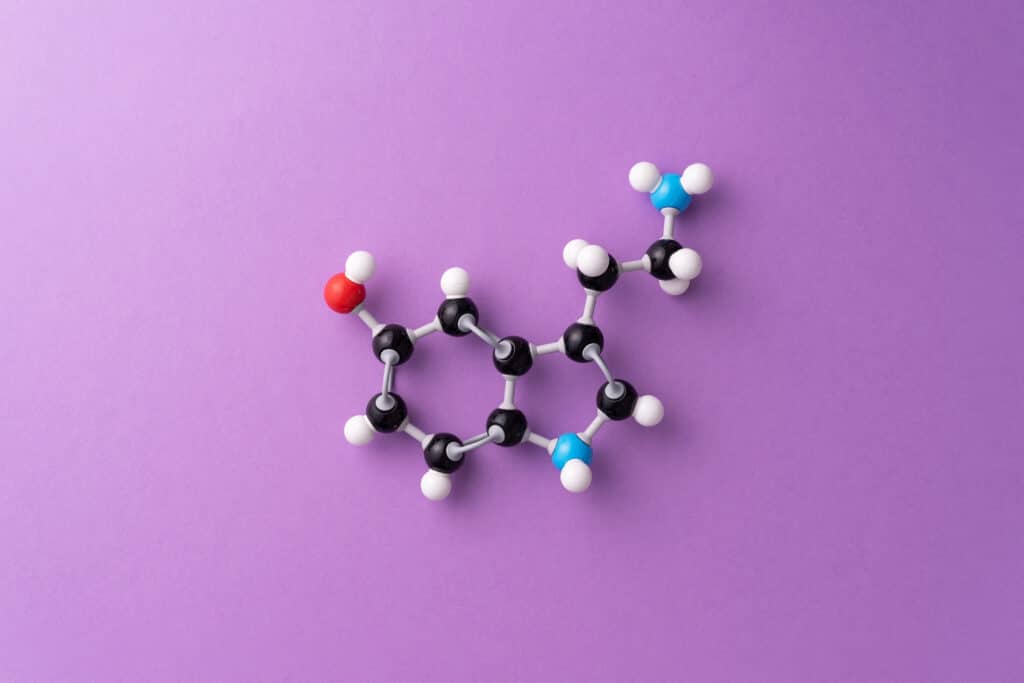
There are many theories about what causes anxiety disorders, and understanding these theories is key to unlocking how to treat a dual diagnosis of substance abuse and anxiety disorder. One of the theories is that the brain’s neurotransmitters (chemical messengers that send and receive neural communications) are out of balance, leaving a person more susceptible to developing an anxiety disorder.
Substance abuse also affects the balance of neurotransmitters, which is important to remember when devising a method of treatment plan for both the anxiety disorder and the addiction.
For example, the neurotransmitter that is responsible for coordinating mood and sleep is serotonin. Reduced levels of serotonin have been associated with anxiety (and depression).
Dopamine, another neurotransmitter, influences pleasure and anticipation of reward. It is targeted by most chemically mood- and mind-altering substances.
Norepinephrine (also known as noradrenaline) is a neurotransmitter that is released as part of the fight-or-flight response that many people with anxiety disorders experience on a frequent or disruptive basis.
Finally, there is GABA, a neurotransmitter that regulates excitement and agitation. It is also produced by the body to induce calm and relaxation.
All these neurotransmitters being out of sync with each other is what contributes to the development of an anxiety disorder and what raises the chances that a person might turn to drugs and alcohol in order to self-regulate their moods. Drugs and alcohol will enact their own chemical influences on these neurotransmitters, deepening the substance abuse and the anxiety disorder, even as the person feels temporary relief from their symptoms and seeks out more.
Detoxification
The first step in treatment for substance abuse and anxiety disorders is breaking the physical dependence that the person has on drugs or alcohol. This process is known as detoxification.
In detox, people are gradually weaned off their normal rate of consumption for mood-altering substances. Abruptly discontinuing intake puts the body through a very difficult process of withdrawal, which many people find unbearably distressful. It can also be quite psychologically harming.
Instead, doctors monitor the process and move the client from one tier of use to a lower tier of use, giving their bodies (and their minds) time to adjust to smaller doses. The British Journal of Clinical Pharmacology writes that a doctor might also prescribe certain medications to ease the transition. Those medications are gradually discontinued as the person continues to adjust to daily functioning without the support of self-medication.
SSRIs
Even with tapered withdrawal, the detoxification process can be very distressing. As the body withdraws from the drugs and alcohol upon which it had become so dependent, people often experience symptoms very similar to those brought on by their anxiety disorder, such as stress, trembling, hyperventilation, irregular heartbeat, and an inability to sleep.
To ease the transition, doctors supervising the detox process might prescribe selective serotonin reuptake inhibitors (SSRIs), anti-anxiety medications that prevent the brain from absorbing the serotonin neurotransmitter. As a neurotransmitter, serotonin sends signals from the brain that are responsible for the coordination of mood and social behavior.
Preventing the brain from reabsorbing serotonin leaves people with an improved mood, enough to guide them through the onset of an anxiety attack. This also helps people navigate the anxiety of withdrawing from drugs and alcohol, so SSRIs are prescribed both for anxiety disorders and detox.
These are examples of selective serotonin reuptake inhibitors:
Fluoxetine (sold under the brand name Prozac)
Sertraline (Zoloft)
Paroxetine (Paxil)
Escitalopram (Lexapro)
Fluvoxamine (Luvox)
Cognitive Behavioral Therapy
In most cases, medical detox lasts for about a week, long enough for the person to be safely past the worst point of their physical cravings for more drugs or alcohol. When medical staff members are satisfied that a period of safety has been reached, the patient will be ready for therapy and counseling to help them control their anxiety and the compulsion to self-medicate.
Cognitive Behavioral Therapy is one of the most popular methods of addressing these concerns. The therapist and the client work together to control the behaviors that channel the anxiety attack. This can cover everything from breathing exercises to counting to 10 when the client notices the signs of an impending anxiety attack.
This same methodology can also help clients control their psychological urges to use drugs or alcohol. Cognitive Behavioral Therapy teaches people how to be aware of the relationships between their thoughts, feelings, and behaviors. The same methods that help people manage their anxiety can help them understand how to focus on positive and healthy thought patterns and behaviors, and rely less on drugs and alcohol to self-medicate.
Family & Group Therapy
None of this is easy, so it requires a lot of time, care, and patience. To facilitate this, the client’s family and close friends might be invited to be part of the treatment. As much as this creates a support and accountability network, it also gives loved ones an understanding of how substance abuse and anxiety disorders work, and what lifestyle or interpersonal changes need to be made for the client’s well-being.
Dialogues in Clinical Neuroscience explains that part of the work involves the client becoming part of group therapy, where they can learn from other people who have a dual diagnosis of substance abuse and anxiety disorder. This kind of support can come in the form of a 12-step program and/or group activities like exercise, yoga, and meditation.
Self-Help: Relaxation & Exercise
Self-help is another option for managing substance abuse and anxiety disorders. Many of the methods used in self-help are derived from those practiced in group therapy settings.
While recovery in a group is the ideal, there will be times a person will not be able to call a sponsor or a friend to help them. They’ll have to get through their anxiety episode or their temptation to relapse on their own. But through therapy, they can have the right tools to deal with the situation
These are examples of self-help approaches for anxiety disorder and substance abuse:
Focused relaxation
This is the practice of methodically tensing and relaxing muscle groups one at a time. This can induce voluntary relaxation when the signs of an anxiety attack are recognized. Experts recommend that you start by clenching and releasing the toes and then continuing up the body.
Exercise
Physical exercise has long been promoted as a simple, easy way to calm nerves and defuse anxiety. As little as 30 minutes a day of walking is enough to redirect some of the symptoms of anxiety when they arise.
Education
Even if a person is not in formal therapy anymore, it can be helpful to read about therapy practices (like how to keep practicing Cognitive Behavioral Therapy techniques) or learn more about anxiety in recovery and disorders or substance abuse to add to the arsenal of self-care. One of the main triggers for relapse is taking recovery and mental health for granted. Staying sharp with self-help skills is a great way to guard against the temptation to return to substance use.
Meditation
This has been practiced for millennia. While there are many benefits to meditating with others, it is also an easy form of self-care to do on your own.There are a number of smartphone apps that block off time for meditating. They play soothing sounds or mantras to draw you into a relaxed state and bring you back out, feeling peaceful and refreshed. People who join a spiritually based 12-step program or a faith community as part of their recovery might think of developing a regular prayer life for similar effects.
Resources & Helplines
If you struggle with substance abuse and anxiety, there is no shame in seeking out resources and helplines. If you need someone to talk to or you’re looking to get connected to a professional treatment program, you can start with any one of these organizations.
National Alliance on Mental Illness (NAMI): 800-950-NAMI (800-950-6264)
Anxiety and Depression Association of America (ADAA): 240-485-1001
National Institute of Mental Health (NIMH): 866-615-6464
American Psychological Association: 800-374-2721
American Psychiatric Association: 800-357-7924
For BIPOC people, there are culturally sensitive organizations that are trained to work with people across language barriers and of differing immigration statuses. The Asian Mental Health Collective serves the Asian, Pacific Islander, and South Asian demographics. The Black Mental Health Alliance offers a directory of Black psychiatrists and doctors. And the Inclusive Therapists organization specializes in offering services to LGBTQ+ and neurodiverse communities.
- What Are Anxiety Disorders? (June 2021). American Psychiatric Association.
- Prevalence and Co-Occurrence of Substance Use Disorders and Independent Mood and Anxiety Disorders. (2004). JAMA Psychiatry.
- Anxiety and Addiction. (2014) Psychology Today.
- Social Anxiety Disorder and Alcohol Abuse. Anxiety and Depression Association of America.
- Alcohol Is a Social Lubricant, Study Confirms. (August 2012). Association for Psychological Science.
- Substance Abuse And Panic-Related Anxiety: A Critical Review. (1990). Behaviour Research & Therapy.
- Substance Use Disorders and Anxiety: A Treatment Challenge for Social Workers. (September 2017). Social Work in Public Health.
- Anxiety Disorders With Comorbid Substance Abuse. (September 2011). Psychiatric Times.
- Addiction and the Brain: The Role of Neurotransmitters in the Cause and Treatment of Drug Dependence. (March 2001). Canadian Medical Association Journal.
- Serotonin Study Explains Why Some People Are More Prone to Anxiety. (May 2020). Inverse.
- Dopamine in Drug Abuse and Addiction: Results From Imaging Studies and Treatment Implications. (April 2004). Molecular Psychiatry.
- Noradrenaline in Mood and Anxiety Disorders: Basic and Clinical Studies. (July 2003). International Clinical Psychopharmacology.
- Neurotransmitters as Food Supplements: The Effects of GABA on Brain and Behavior. (October 2015). Frontiers in Psychology.
- Neurotransmitters, Psychotropic Drugs and Microglia: Clinical Implications for Psychiatry. (2013). Current Medicinal Chemistry.
- Pharmacological Strategies for Detoxification. (February 2014). British Journal of Clinical Pharmacology.
- Medication Options. (July 2019). Anxiety and Depression Association of America.
- Serotonin and Mental Disorders: A Concise Review on Molecular Neuroimaging Evidence. (2014). Clinical Psychopharmacology and Neuroscience.
- The Role of Selective Serotonin Reuptake Inhibitors in Preventing Relapse of Major Depressive Disorder. (January 2018). Therapeutic Advances in Psychopharmacology.
- Cognitive-Behavioral Therapy for Panic Disorder in Patients Being Treated for Alcohol Dependence: Moderating Effects of Alcohol Outcome Expectancies. (Jun-July 2009). Addictive Behaviors.
- 3 Easy Anxiety Relief Exercises You Can Use Anywhere. (January 2017). University of Michigan Health.
- Beyond Worry: How Psychologists Help With Anxiety Disorders. (October 2016). American Psychological Association.
- Substance Abuse Treatment and Family Therapy. (2004). Center for Substance Abuse Treatment.
- Cognitive Behavioral Group Therapy for Anxiety: Recent Developments. (September 2015). Dialogues in Clinical Neuroscience.
- Self-Care for Anxiety and Depression: A Comparison of Evidence From Cochrane Reviews and Practice to Inform Decision-Making and Priority-Setting. (August 2020). BMC Complementary Medicine & Therapies.
- Effects of Exercise and Physical Activity on Anxiety. (April 2013). Frontiers in Psychiatry.
- Anxious? Meditation Can Help You ‘Relax Into the Uncertainty’ of the Pandemic. (May 2020). NPR.
















