Hydrocodone is an opioid painkiller prescribed to treat moderate to severe pain. However, some people misuse it to get high. Whether you take it for a medical purpose or abuse it, chronic use can lead to physiological dependence, which means you will experience unpleasant hydrocodone withdrawal symptoms if you abruptly stop taking it.
Hydrocodone withdrawal symptoms can last between 10 to 20 days, depending on the hydrocodone format you’re using.[1]
| Short-Acting Hydrocodone | Long-Acting Hydrocodone | |
| When does it start? | 8–24 hours | 12–48 hours |
| When does it end? | 4–10 days | 10–20 days |
Hydrocodone Withdrawal Symptoms
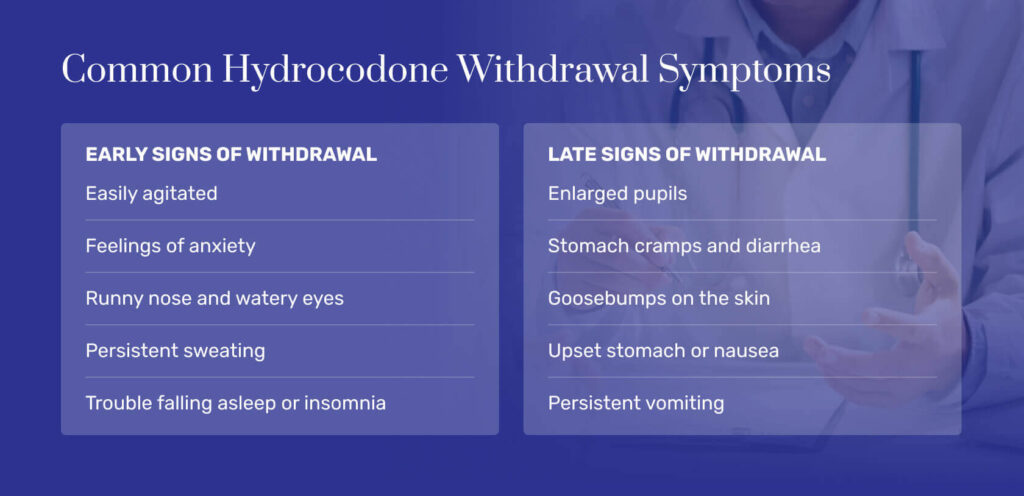
Opioid withdrawal is considered a life-threatening condition that stems from drug use.[2] With repeated use, your brain becomes accustomed to the drug. If you quit suddenly, you can feel physically and mentally ill. Symptoms can be split into early and late stages.[3]
Early signs of opioid withdrawal include the following:[3]
- Agitation
- Anxiety
- Aching muscles
- Watery eyes
- Insomnia
- Runny nose
- Sweating
- Yawning
Late signs of opioid withdrawal include the following:[3]
- Stomach cramps
- Diarrhea
- Enlarged pupils
- Goosebumps
- Nausea
- Vomiting
Severe symptoms can be dangerous. Relentless vomiting and diarrhea can lead to dehydration and organ damage. And persistent muscle weakness and anorexia could leave you feeling too weak and unhappy to nourish your body.
Hydrocodone Withdrawal Timeline: What to Expect
Multiple forms of hydrocodone exist, and they persist in the body for different time frames. Knowing if your medication is a short-acting or long-lasting form of the drug is important.
A short-acting hydrocodone medication is made to work quickly and fade away fast. Your acute withdrawal symptoms could appear within 8 to 24 hours of your last dose. Without treatment, they could last between 4 and 10 days.[1]
Short-Acting Hydrocodone
| Time Since Last Use | Symptoms | Symptom Intensity |
|---|---|---|
| 8-24 hours | Opioid cravings, anxiety, muscle aches, stomach cramps, runny nose, tearing, sweating, yawning | Mild to moderate |
| 3-4 days | Rapid heart rate, increased blood pressure, severe anxiety, depression, chills, vomiting, diarrhea, and goosebumps | Symptoms peak in severity |
| 7-10 days | Mild depression, moderate anxiety, moderate cravings, and runny nose | Symptoms begin to resolve |
Extended-Release Hydrocodone
A long-lasting hydrocodone medication is designed to offer extended relief. Your acute withdrawal symptoms could begin between 12 to 48 hours, and they could last 10 to 20 days.[1]
| Time Since Last Use | Symptoms | Symptom Manifestation |
|---|---|---|
| 12-48 hours | Cravings, yawning, anxiety, muscle pain, stomach cramps, runny nose, tearing, sweating | Mild to moderate |
| 6-8 days | Severe anxiety, severe depression, hypertension, rapid heart rate, chills, vomiting, diarrhea, and goosebumps | Symptoms peak in severity |
| 14-20 days | Moderate opioid cravings, moderate anxiety, mild depression, and runny nose | Symptoms begin to improve |
Post-Acute Withdrawal Symptoms
Once acute hydrocodone withdrawal resolves, people may experience milder symptoms for an extended period of time—even up to a year after quitting. These are known as protracted withdrawal symptoms or post-acute withdrawal symptoms, and they can be a significant risk factor for relapse.
Common protracted withdrawal symptoms associated with opioid dependence include:[6]
- Depression
- Anxiety
- Sleep disturbances
- Fatigue
- Emotional blunting or inability to feel pleasure
- Irritability
- Reduced ability to focus
- Issues with executive control functions like planning and executing
These symptoms can fluctuate, disappearing for a while and then returning during times of stress. Because of these lingering symptoms, it’s important to receive ongoing support, including therapy, support groups, and step-down care.
Factors That Affect Hydrocodone Withdrawal Severity & Duration
Your drug’s formulation has a deep impact on your withdrawal experience. But other factors can change how you feel and how long the discomfort lasts. Some of these issues you can change, and others you can’t.
Your hydrocodone withdrawal severity and duration could be impacted by the following factors:
- Organ health: If your liver and kidneys aren’t working properly, it’s harder to remove drugs from your system.
- Mixing: If you add other drugs to your doses, your withdrawal symptoms may vary and last longer.
- Age: Older people tend to need more time to process drugs than their younger counterparts.
- Physical health: Underlying conditions like diabetes, cancer, and gastrointestinal disease could make your symptoms harder to tolerate.
- Mental health: Anxiety, depression, and other concerns could make ignoring your symptoms harder.
- Length of abuse: The longer you’ve misused drugs, the more accustomed every cell in your body is to those substances. Quitting could be harder as a result.
- Genetics: Some people process opioids faster due to their genetic makeup. Their withdrawal process might move faster because of this.
Treatment for Hydrocodone Withdrawal: Medical Detox
Hydrocodone withdrawal isn’t just uncomfortable. It can also be life-threatening. The more frequently you attempt withdrawal and relapse, the harder your next attempt will be. Medical detox can help.
A medical detox program involves getting care 24 hours per day in an inpatient or hospital setting. A care team provides you with medications to ease withdrawal symptoms. Your team uses food, fluids, therapy, and support to help you move through the process safely and comfortably.
Medical detox alone is not a treatment for opioid addiction. But it can help you get sober and healthy, so you can focus on the next steps of your journey to long-term recovery.
Medications for Hydrocodone Withdrawal
Opioid withdrawal involves using prescription medications to correct chemical imbalances and repair the damage long-term drug use has caused. Multiple options are available.
To address your opioid addiction specifically, your team might use one of the following medications:[3]
- Methadone: This FDA-approved medication latches to opioid receptors, mimicking their action without making you high.
- Buprenorphine: The FDA has also approved this weak opioid agonist to ease withdrawal symptoms and drug cravings.
Your team may also use medications to ease your withdrawal symptoms. Typically, these options are used in conjunction with FDA-approved drugs that target opioid addiction specifically.
Those additional medications include the following:[2],[3]
- Loperamide: This medication can ease diarrhea, so you won’t feel so dehydrated.
- Promethazine: This medication reduces vomiting, so you can eat good meals and keep them down.
- Ibuprofen: This medication can lessen pain from headaches and sore muscles.
- Clonidine: This medication lowers your blood pressure, so you feel more like yourself.
Post-Detox Opioid Addiction Treatment
At the end of a detox program, you’ll have no drug remnants in your system. But you’ll need more help to stay sober for good. A quick transition to a qualified hydrocodone treatment program is the last part of your detox plan.
In a hydrocodone addiction treatment program, you’ll access counseling and therapy to help you build sober habits. And you’ll use therapies like meditation, nutrition, and exercise to heal your body and slow your mind.
The following two major treatment settings exist:
- Inpatient treatment: You move out of your home and into a treatment program. Partial hospitalization programs (PHPs) offer the most intense form of inpatient care, but others can be just as helpful.
- Outpatient treatment: You live at home while getting care. A standard outpatient program might require just a few hours of time per week. But an intensive outpatient program (IOP) means getting therapy for the majority of every day, most days of the week.
No matter what form of care you get, you’ll work on your long-term recovery with qualified professionals. With their help, you will gain control of your life and get better.
Frequently Asked Questions About Hydrocodone Withdrawal
We’ve compiled some of the most common questions about hydrocodone withdrawal.
Hydrocodone withdrawal lasts between 4 and 20 days, depending on the drug formulation you used. Withdrawal timelines will vary depending on whether you use medication-assisted treatment or stop taking hydrocodone cold turkey.
Severe dehydration caused by hydrocodone withdrawal can be life-threatening. If you relapse to drugs during withdrawal to get relief, you can die from an overdose. Overdose is more likely if you relapse after your opioid tolerance has lessened.
Enter a medical detox program and use medications to help your brain heal. This method is safe, effective, and can result in a lifetime of sobriety. Studies show you are more likely to maintain recovery if medications like buprenorphine are used.[4]
- Withdrawal management. Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings. Published 2009. Accessed August 31, 2023.
- Shah M, Huecker M. Opioid withdrawal. StatPearls. Published April 29, 2023. Accessed August 31, 2023.
- Opiate and opioid withdrawal. U.S. National Library of Medicine. Published April 30, 2022. Accessed August 31, 2023.
- Maglione MA, Laura R, Christine C, et al. Effects of medication-assisted treatment (MAT) for opioid use disorder on functional outcomes: A systematic review. Rand Health Q. 2020;8(4):RR-2108-OSD. Published 2020 Jun 15
- Opioid withdrawal symptoms, a consequence of chronic opioid use and opioid use disorder: Current understanding and approaches to management January 2020.
- Protracted Withdrawal. Substance Abuse and Mental Health Services Administration.



