What Is Cymbalta Withdrawal & Why Does It Happen?
Cymbalta withdrawal involves symptoms that appear when you abruptly stop taking this medication. It’s a common issue. People who quit duloxetine (the generic version of Cymbalta) may experience symptoms like headache, nausea, and dizziness when they quit.
Are you or someone you know struggling with addiction?
I may have a problem I am concerned for a loved oneSerotonin-Norepinephrine Reuptake Inhibitor (SNRI) medications like Cymbalta act on serotonin and norepinephrine receptors within the brain. Their action can decrease symptoms caused by major depressive disorder, anxiety disorder, mental illness and chronic pain.
People take Cymbalta once per day at doses between 30 mg and 120 mg. In time, their brain cells become accustomed to the medication—known as dependence. Physical dependence is a normal and natural reaction to the constant presence of drugs and doesn’t mean the person is addicted.
However, when you develop physical dependence, your brain cells will not function properly without Cymbalta. Suddenly stopping this medication will lead to Cymbalta withdrawal symptoms, also known as “antidepressant discontinuation syndrome.” You should talk to your doctor about gradually tapering off this medication, which can reduce the risk and severity of withdrawal. If you need professional support during this process, a Florida detox center can provide medical detox and safe medication tapering under clinical supervision.
Cymbalta Withdrawal Symptoms
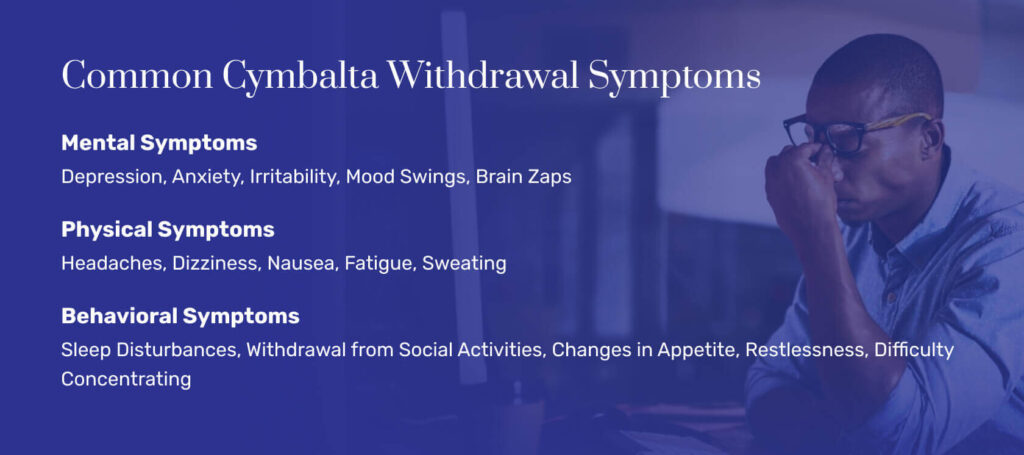
If you’ve taken Cymbalta for long periods, your body believes it needs the drug. When you quit suddenly, withdrawal begins. In severe cases, people who quit Cymbalta abruptly develop the following symptoms:
Mental health
Depression, irritability, anxiety, confusion, and agitation are often associated with Cymbalta withdrawal.
Physical health
Detoxing from Cymbalta can lead to headaches, dizziness, lethargy, flu-like symptoms, and gastrointestinal distress. Some people feel a shocking sensation in their fingers and toes. Others report an uptick in energy and even episodes of mania. Some people even develop seizures during their withdrawal process, and those episodes can be life-threatening.
Behavioral health
People who are withdrawing from Cymbalta might experience disturbances in their sleep or changes in their appetites. They may also seem withdrawn or show less interest in activities they used to enjoy. Other behavioral changes include restlessness and difficulty concentrating.
Withdrawal symptom severity can vary based on how much of the drug you took, how long you were exposed to Cymbalta, and your overall health.
Cymbalta Withdrawal Timeline
There is no boilerplate schedule for Cymbalta withdrawal as every person and every body is a little different. You should never try to quit Cymbalta cold turkey. Always work with a medical team to develop a tapering schedule, and follow your team’s recommendations carefully.
Your doctor can help you craft an appropriate plan based on your unique needs, including your mental health symptoms and how high of a dose you were on.
This is a common duloxetine withdrawal timeline for people who quit the drug abruptly:
Week 1: Begin to Taper
Flu-like symptoms (lethargy, headache, aching) accompanied by nausea develop.
Week 2: Continue to Taper
Symptoms continue and are accompanied by anxiety, irritability, and aggression.
Week 3: Taper to Minimum
Symptoms begin to fade.
Week 4: Complete Detox
Flu-like symptoms and pain are gone, but you may still experience lingering mental health challenges. Before long, you should feel like yourself.
Tapering Off Cymbalta
Never try to quit Cymbalta cold turkey. Always work with a medical team to develop a tapering schedule, and follow your team’s recommendations carefully.
Each person needs a different tapering schedule. A timeline that works for you could be wrong for someone else. Your doctor can help you craft an appropriate plan based on your unique needs, including your mental health symptoms and how high of a dose you were on.
A sample Cymbalta schedule may look like this:
| Day 1 | You take less Cymbalta than you did previously. |
| Day 3 | You continue to taper and develop moderate issues, such as restlessness and insomnia. |
| Day 6 | Your taper continues, and your symptoms get slightly more severe. You may have gastrointestinal symptoms in addition to mental health challenges. |
| Week 2 | You continue to taper, and you notice that your discomfort is fading. |
| Week 3 | You’re barely taking any Cymbalta, and you feel like yourself. |
Since withdrawal from Cymbalta can be so variable, it’s critical to work with a team that can support you, monitor progress, and offer help when needed.
Tips for Tapering Off Cymbalta
It’s critical to care for yourself while quitting Cymbalta. Your discomfort will fade as your taper progresses. But self-care can keep you comfortable as your body adjusts.
The following tips may help:
Gather support. Tell your family and friends you’re working with your doctor to quit Cymbalta. Ask for their help and patience as you adjust.
Nourish your body. Stay hydrated. Fill your plate with healthy foods you enjoy.
Redirect your attention. Read, garden, or do something you enjoy. Focusing on your symptoms can make you feel worse.
Try mind/body approaches. Meditation and yoga can help you feel grounded and connected with your body.
Use exercise. If you feel strong enough, try a workout. You’ll boost natural feel-good chemicals each time you move or stretch.
Stay in touch with your doctor during the taper. If you’re still uncomfortable while following these detox tips, your doctor may need to offer more assistance.


Treatment for Cymbalta Addiction
Professional Treatment for Cymbalta Detox
If you’re using Cymbalta as prescribed, you do not need a professional detox program—you just need to work with your doctor to wean off the medication. But if you abuse Cymbala, you may benefit from addiction treatment.
While antidepressant abuse isn’t common, researchers say it’s possible. Some people take large doses of drugs like Cymbalta for their stimulant effects. Someone like this may develop a Cymbala addiction and need detox services.
In a detox program, teams can taper your dose properly and offer therapies for uncomfortable side effects. This is a safer way to get sober. Once the program is complete, you can enter rehab programs to preserve your newfound sobriety.
If you’re ready to begin long-term recovery, an Indiana alcohol and drug rehab provides structured therapy and ongoing support after detox.
Your detox options include the following:
Hospitalization
If you’ve abused multiple substances or your seizure risk is high, a medical detox hospital-based program may be the right setting. You’ll get around-the-clock care.
Inpatient care
In an inpatient detox program, you’ll work with counselors and therapists to taper. It’s an appropriate model for people who can’t get sober at home but who don’t have significant underlying health problems.
Outpatient treatment
You work with a treatment team in a series of appointments, but you conduct an unsupervised taper at home.
Detoxing safely is part of a treatment program, but it’s not the end of one. Once you’re sober, you still face all of the triggers and challenges that made you abuse Cymbalta in the first place. A treatment program can help.
In a structured addiction treatment program, treatment professionals can help you build up the skills to deal with old triggers in new ways. You’ll emerge with a toolkit you can use when you’re tempted to abuse Cymbalta. And you’ll understand what you must do to keep yourself healthy and sober.
Talk to your doctor about addiction treatment, and enroll in a program that’s right for you. With the right support, you can build the foundation for a balanced life in recovery.
Cymbalta Withdrawal & Detox Frequently Asked Questions
We’ve compiled common questions about Cymbalta withdrawal and detox.
If you quit Cymbalta cold turkey, you could experience life-threatening symptoms for two weeks or longer. If you quit with a taper, your systems may be mild and last for several weeks.
Work with a doctor and develop a tapering schedule. You’ll reduce the severity of withdrawal symptoms with this method.
Benadryl is a sedating antihistamine. Some people find the medication helps them to sleep. But if you’re using Cymbalta, even in a taper, don’t mix your medication with anything without asking your doctor first. Follow their instructions on how to proceed.
Wellbutrin is an antidepressant, like Cymbalta, but it’s in a different medication class. Never mix prescription medications like Wellbutrin with Cymbalta without asking your doctor first. Experts say you should stop SSRIs like Cymbalta before starting another antidepressant like Wellbutrin.[4]
If you or someone you know is struggling with Cymbalta withdrawal or needs support in tapering off, we’re here to help. Contact us today to explore safe and effective treatment options tailored to your needs.
- Cymbalta prescribing information. U.S. Food and Drug Administration. U.S. Food and Drug Administration. Published October 2010. Accessed July 8, 2023.
- Gabriel M, Sharma V. Antidepressant discontinuation syndrome. CMAJ. 2017 May 29;189(21):E747. doi: 10.1503/cmaj.160991. PMID: 28554948; PMCID: PMC5449237.
- Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014 Aug 14;5:107-20. doi: 10.2147/SAR.S37917. PMID: 25187753; PMCID: PMC4140701.
- Appendix D: Switching antidepressants. BC Guidelines. Published 2013. Accessed July 8, 2023. BC Guidelines. Published 2013. Accessed July 8, 2023.
















