Are you or someone you know struggling with addiction?
I may have a problem I am concerned for a loved oneAddiction is a chronic condition that affects the brain and body—it’s characterized by compulsive substance use despite negative consequences. Many substances can trigger addiction, including alcohol, opioids, benzodiazepines, stimulants, and marijuana. Factors such as family history, genetics, environment, and more can increase your risk.
While addiction is a chronic condition that can’t be cured, treatment can help manage it. Evidence-based therapies can help you manage drug use triggers and make relapse less likely.
What Is Addiction?
Quick Answer
The American Society of Addiction Medicine defines addiction as a chronic, treatable medical disease that involves the brain, genetics, the environment, and a person’s life experiences.[1]
Addiction, also known as a substance use disorder (SUD), begins with drug experimentation. Brain chemical and circuitry changes caused by that abuse make drug use compulsive, not voluntary. Someone might choose to use drugs or alcohol the first time, but when addiction develops, they lose control over their continued use.
While addiction is a chronic condition that never disappears, it’s treatable. Evidence-based techniques can help people overcome changes caused by drug use so they can lead healthy, productive lives.
Key Facts About Addiction
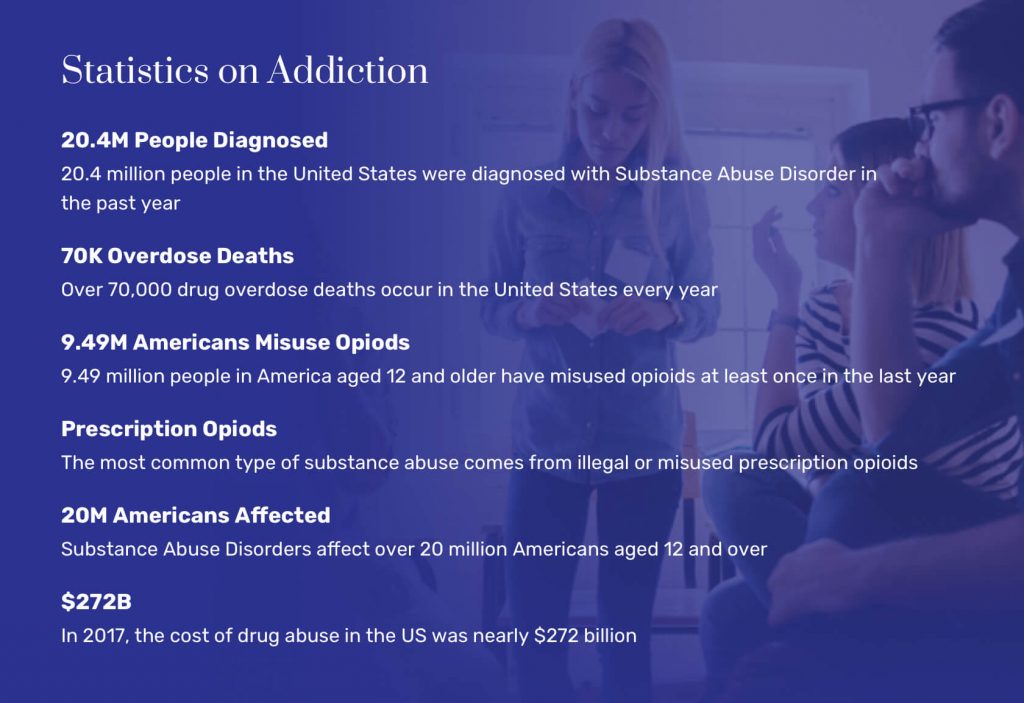
- The annual economic impact of alcohol abuse is $249 billion, while the annual impact of illicit drug use is $193 billion. [2]
- An estimated 21 million Americans have drug or alcohol addiction. [3]
- Almost 83,000 drug overdose deaths were caused by opioids in 2022. Drug overdose statistics linked to other substances are similarly alarming. [4]
- Overdose deaths caused by synthetic opioids like fentanyl rose 16% between 2018 and 2019.
- Nearly a quarter of Americans had some form of mental illness in 2020. Depression and addiction are closely linked, as are anxiety disorders and personality disorders.
- Experts say America is in the grip of an “opioid epidemic” causing waves of overdose deaths. [5]
Is Addiction Considered a Disease?
The National Institute on Drug Abuse (NIDA) defines addiction as a disorder, not a disease. Experts say that addiction is similar to other diseases (including heart disease), but they are careful to use the word disorder when defining substance abuse. [6]
Medical experts reserve the word disease for conditions that have an underlying cause but are involuntary physiological or biological illnesses. A disorder, on the other hand, is a collection of signs and symptoms that are somehow related. [7]
What Are the Causes of Addiction?
Why do some people develop SUD and others do not? The causes of addiction are complex, and they often overlap. The more factors you have, the more likely it is that you’ll struggle with compulsive drug use if you experiment with drugs.
Three main risk factor classifications exist.
Biological
Researchers say between 40% and 60% of a person’s addiction risk is caused by genes. [6] Those factors can include the following:
- Inherited mental health concerns: Problems like depression or anxiety can run in families. Those issues can increase SUD risks too.
- Inherited drug reactions: Some people have stronger responses to drugs, making an addiction more likely.
- Inherited processing speed: Some people can metabolize drugs faster or slower, increasing addiction risks.
Physiological
Your body processes each dose of drugs you take. Sometimes, your physiological makeup and drug use method increase your SUD risks. Physiological factors can include the following:[6]
- Drug use methods: Using drugs via needles exposes brain cells to drugs almost immediately. The damage this method can cause could increase addiction risks.
- Organ health: Quick drug metabolization without nasty side effects could make drug use more pleasurable and addiction more likely.
- Brain responses: Some people have stronger reactions to drugs, and damage to brain cells happens more quickly for them.
- Early drug use: Adding drugs to a growing brain can lead to quick SUD progression. The younger you are when you start using drugs, the higher the likelihood of addiction.
Environmental
Where you live, how you were raised, and other environmental factors could increase your addiction risks. These environmental factors can include the following:[6]
- Family habits: Growing up with parents who drink or use drugs could normalize the behavior and allow for early substance use.
- Easy access: Living in neighborhoods where drug use is common could enable you to buy drugs easily.
- Peer pressure: If your housemates, friends, and colleagues use drugs, you are more likely to do the same.
Common Signs & Symptoms of Addiction
People who struggle with an addiction might exhibit various behaviors, including the following:
- Taking more of the drug in one evening or event than intended
- Taking the drug for longer than intended
- Trying to quit but being unable to
- Intense cravings for the drug until it is all you can think about
- Giving up other activities to become intoxicated
- Continuing to consume the substance despite health and social consequences
- Experiencing physical or psychological problems because of intoxication, like worsened depression or anxiety
- Having problems at work, with school, or in your personal life because of intoxication
- Getting into dangerous situations, like driving while intoxicated
- Lying to friends and family about substance use, stealing substances from them, or stealing to get more of the drug
- Developing a tolerance, or feeling the need to take more of the drug to get the original high
- Developing a dependence on the drug, or feeling the need to take the drug to feel normal
- Experiencing withdrawal symptoms when not taking the drug
- Beginning to use multiple substances, such as alcohol and marijuana
What Are the Typical Stages of Addiction?
Addictions don’t develop overnight. Instead, most people with SUD progress through a series of recognizable and understandable steps. Knowing the stages of addiction is critical, as it can allow you to get help early.
Stage 1: Experimentation
During the experimentation stage, someone chooses to drink or use drugs for the first time. If that experience is pleasant, the person may repeat it.
Example: Sarah is offered alcohol at a party, and she decides to try it.
Stage 2: Social/Regular
During this stage, a person’s drug use increases. They may lean on party situations to continue their substance use, or they may begin using the drug independently.
Example: Sarah always asks if alcohol will be available before she will go to a party. She buys beer for at-home, personal use.
Stage 3: Problematic Use
As drug use deepens, people begin using drugs frequently. Sometimes, they use drugs in dangerous situations that could cause long-lasting problems.
Example: Sarah starts adding whiskey to her morning coffee. She’s often drunk when she drives into the office parking lot.
Stage 4: Tolerance
With continued drug use, brain cells adjust. People need larger doses to bring about the intoxication smaller amounts once delivered.
Example: Sarah’s nightly beer no longer gets her intoxicated. She switches to vodka instead and now drinks several martinis each night.
Stage 5: Dependence
Brain cells no longer function properly without drugs. People feel sick between doses, and their drugs may not make them feel high.
Example: Sarah needs a martini in the middle of the night to stop her hands from shaking. That drink doesn’t make her feel drunk.
Stage 6: Addiction
Addiction is a mental health disorder characterized by compulsive use. At this stage, people put substances at the center of their lives and make all decisions related to whether they can access the drug.
Example: Sarah keeps her home fully stocked with alcohol. She doesn’t meet friends, keep her volunteer appointments, or do anything that doesn’t involve drinking.
Stage 7: Relapse
A relapse is a return to drug use after a period of sobriety. A relapse is not a failure, but it implies that the person needs more help and treatment.
Example: Sarah emerges from a 30-day detox facility and has a difficult day at work. She drinks a martini and immediately regrets it. She calls her therapist for help.
Long-Term Impact of Addiction
People with addiction may spend weeks, months, or even years before getting the help they need. They may face health and personal side effects due to their substance abuse.
Health Impact
Specific health challenges are closely related to the drugs people use. But NIDA says addiction is often linked to the following health problems:[8]
- Heart disease
- Lung disease
- Stroke
- Cancer
- Mental health disorders
- Infections, such as HIV and hepatitis C
Impact to Life
Untreated SUD can also touch almost every part of your life. Common challenges include the following:
- Job loss
- Loss of savings, including retirement accounts
- Homelessness
- Lack of family and friends
- Loss of custody of children
Addiction & Dual Diagnosis
SUD and mental health conditions often co-exist. Researchers say 17 million American adults had both mental illnesses and SUD in 2020. [9]
Some people use substances to help control their mental health symptoms. Others develop mental health challenges due to substance use. When addiction and SUD develop together, it’s called a dual diagnosis.
Conditions often associated with SUD include the following:
- Depression: More than a blue mood, depression can cause deep distress and feelings of inadequacy and loss.
- Anxiety disorders: Significant anxiety can leave people feeling worried about almost every part of their lives.
- ADHD: Attention deficit hyperactivity disorder (ADHD) can lead to compulsive behaviors, including substance abuse.
- Bipolar disorder: People with bipolar disorder often experience significant and troubling mood swings.
- Personality disorders: People with personality disorders often struggle to form healthy relationships with others. Their isolation may lead to SUD.
- Eating disorders: Anorexia, bulimia, and other eating disorders are often closely related to substance abuse.
Different Types of Addiction
Different types of addiction are grouped based on the main substance of abuse. Sometimes, people abuse multiple intoxicating substances, like smoking and drinking alcohol, but often, one of these drugs is the main craving or compulsion.
Categories of substance abuse include the following:
Alcohol Use Disorder
Also called alcoholism or alcohol addiction, alcohol use disorder is one of the most common addictions. Alcohol is one of the most prevalent problematic drugs in the world.
Although drinking alcohol is socially acceptable, this intoxicant can cause a release of neurotransmitters that cause relaxation, sleepiness, and euphoria. Excessive or problem drinking is common in many countries. Becoming dependent on alcohol to feel better may lead to addiction.
Cannabis Use Disorder
As marijuana becomes more socially acceptable in the United States, more people are abusing this drug as they would abuse alcohol. Similarly, this substance can lead to relaxation and euphoria, although marijuana also has some hallucinogenic properties.
Like alcohol, it is possible to become dependent on cannabis without becoming addicted, but dependence can lead to escalating use, which can be a sign of marijuana addiction.
Hallucinogen Use Disorder
Hallucinogenic drugs alter one’s perception of the world by flooding the brain with neurotransmitters. There are many types of hallucinogens, including LSD, ketamine, shrooms, DMT, PCP or “angel dust,” ibogaine, and, increasingly, research chemicals. Some hallucinogens occur in nature, while others are made in a laboratory.
While hallucinogens are not considered addictive, it is possible to abuse them to the point that the brain becomes tolerant to them and might crave them compulsively to feel normal. In recent years, microdosing hallucinogens to get a mild high has become trendy. This can cause an addiction to hallucinogens, as the person quickly needs more than a small dose.
Inhalant Use Disorder
Sniffing glue, huffing paint, and whippits are comedic tropes in pop culture, but these activities are extremely dangerous. While some volatile chemicals can cause a mild euphoric effect, this does not last long.
The substances are much more likely to cause other problems, including heart irregularities, stroke, brain damage, and psychosis. An addiction to inhalants can develop quickly.
Opioid Use Disorder
Opioid addiction can lead to overdose, which is one of the most common causes of drug-related death in the U.S. The most drugs underlying opioid addiction in this modern epidemic are prescription painkillers.
At a certain point, a person may no longer receive a prescription for painkillers. If the individual cannot taper their use, they may begin to steal other prescription opioids from friends and family or find counterfeit versions on the black market. This often leads to heroin addiction as well as fentanyl abuse and overdose.
Stimulant Use Disorder
There are several types of stimulants, from prescription to illicit. Drugs like Adderall, Ritalin, cocaine, crystal meth, and others are all very addictive. While prescription stimulants have legitimate uses with oversight from a medical professional, people who do not need these drugs and try them for fun are at risk of becoming addicted.
Stimulants create a high-energy euphoria. When this wears off, the person may feel tired, grumpy, sad, or anxious. Stimulants and addiction are closely related.
Benzodiazepines & Other Sedatives
Although some sedatives, like alcohol and marijuana, are obvious intoxicants, there are many prescription sedatives that can become addictive too. Sleep aids like Ambien and anti-anxiety medications like Xanax are currently the most common. These drugs have a similar effect on the brain as alcohol, leading to a sense of relaxation and well-being.
The body can also quickly become tolerant to benzodiazepines and sedatives with regular use, meaning the person may feel the need to take more than prescribed to get the original effects. The person may also take the drugs recreationally rather than for medical reasons. This can lead to benzodiazepine addiction.
Other Substances of Abuse
Research chemicals like bath salts or synthetic marijuana, kratom, new prescription medications based on opioids or stimulants, steroids, clonidine, and combinations of drugs like MDMA and caffeine can cause intense highs that lead to addiction.
What Are the Most Commonly Abused Substances?
Many substances are available within the United States, and many of them are closely related to SUD.
These are substances known to spark SUD in some people:[10],[11],[12],[13],[14]
- Alcohol: More than 140,000 people died of alcohol-related causes from 2015 to 2019.
- Cannabis: About 30% of people who use marijuana may have some degree of marijuana use disorder.
- Hallucinogens: Weeks or months after use, some people develop terrifying flashback memories of their substance use.
- Opioids: Nearly 75% of drug overdose deaths in 2020 involved an opioid.
- Stimulants: Several stimulants have no medical use in the United States, but some (like Ritalin) are available via prescription.
- Sedatives: The sedative drug class is large and includes sleep aids, antidepressants, and more.
- Inhalants: People rarely think of inhalants as dangerous, but they can lead to significant problems.
Bath salts/synthetic marijuana: While some states have moved to ban synthetic drugs, including bath salts, manufacturers respond by changing formulations. With continual alterations, they often manage to stay one step ahead of the law.
Comparing Substance Use Disorders
While many substances can spark SUD issues, the risks and harms are different.
| Substances | Abuse Potential | Overdose Potential | Overdoses per Year, Avg. | Statistics/Examples |
| Alcohol | High | High | 2,200 | Most people who die from alcohol poisoning are between the ages of 35 to 64. |
| Cannabis | Moderate | Low | None | In 2015, 138,000 people voluntarily sought treatment for marijuana use. |
| Hallucinogens | Moderate | Very low | None | LSD, psilocybin, PCP, ketamine, MDMA |
| Opioids | High | High | 69,000 | Heroin, fentanyl, synthetic opioids, Dilaudid, Percocet, kratom |
| Stimulants | High | High | About 53,000 | Cocaine, crystal meth, crack, Adderall |
| Sedatives | High | High | More than 9,500 (benzodiazepines only) | Xanax, Ambien |
| Inhalants | High | High | Very low (often attributed to other sources) | Whippits, aerosols, solvents, nitrates, gases |
Common Myths About Addiction
Myths about addiction can keep people from getting the help they need. Combating them is an important part of supporting someone who is dealing with substance abuse.
These are three common myths associated with addiction:[16]
- Willpower alone can cure addiction. In reality, SUD begins with brain chemistry changes. Many people need medications to help them stop abusing drugs. There is no cure for addiction, but it can be successfully managed.
- Addiction is lifelong. SUD is a chronic condition, but many people find helpful ways to address their cravings in treatment, and they avoid relapse risks. You can manage your addiction for the rest of your life.
- People must hit rock bottom before they can get help. People with addictions can start a new life at any point, even if their lives are still functional. People seek out recovery at various points in life.
Evidence-Based Treatment for Addiction: 3 Steps
It is important to remember that addiction is a treatable condition. Several components can be part of the process, depending on individual needs.
Step 1: Medical Detox
This is the first step in the treatment process, when the body can overcome its dependence on the substance. For people with mild or moderate addictions, it is possible to go through detox with medical oversight and supportive therapies like nutritional supplements and exercise. This typically takes one to two weeks, depending on the substance.
Many medical professionals advocate for various types of medication-assisted treatment (MAT), or using a prescribed medication to help the person taper the body off the need for drugs. Those medications include buprenorphine, methadone, and combination therapies (like Suboxone). Medical detox can be very effective.
Step 2: Rehabilitation
The next step in the recovery process is rehabilitation, which centers around therapy. For most recovery programs, group therapy is the focus, but many programs are beginning to offer individual therapy too.
Other therapies include animal therapy, art therapy, yoga, nutrition therapy, occupational and physical therapy, speech therapy, and family support therapy. Since different programs offer different approaches, the experience should be tailored to individual needs.
Your rehabilitation program can take place in different settings, including the following:
Step 3: Aftercare
At the end of rehabilitation, you may develop a plan to support yourself if you become stressed or experience triggers for relapse. This includes avoiding certain neighborhoods and keeping a list of safe people to call. It should also include positive events like a daily schedule; motivational and inspirational details like art, podcasts, books, or movies; an exercise routine; and new hobbies that do not involve substance abuse.
Alongside rehabilitation and aftercare, many recovery programs are now also offering additional support like job training, book clubs, help finding housing and resources, and even help finding post-rehabilitation programs like sober housing or mutual support groups.
Things to Consider When Looking for Addiction Treatment
When looking for a good program, here are some things to consider in addition to individual needs:
- Accreditation: Local, state, and federal health agencies offer different certifications. Make sure the recovery program has medically trained staff and is certified at the state level.
- Evidence-based treatment: Using the guide above, ask the program how they approach detox and rehabilitation. Programs that claim very high success rates or “cures” for addiction are not based on medical science. There is no cure for addiction, though it can be managed on a long-term basis.
- Family support: Family members and close friends are vital to ongoing recovery. Staying balanced means maintaining healthy connections with these individuals. This may mean attending family therapy as well as ensuring the program offers regular communication through letters or visits, or that families are included in other ways in the treatment process.
- Continuing care: Most programs recognize that chronic illness means a lifetime of support, so they offer ongoing support through aftercare planning and other resources. Continued family involvement, access to outpatient support groups, a tiered plan for care, and other approaches all recognize that treatment can take time, without restricting the person’s life.
Support Resources for Addiction
These organizations could be helpful as you look for a new life in sobriety:
- Alcoholics Anonymous: Find peers also struggling with substance use, and learn from them.
- Al-Anon: Join support groups that are made for people with loved ones who are dealing with addiction.
- National Institute on Drug Abuse: Tap into research on how addictions work and are treated.
- Substance Abuse and Mental Health Services Administration: Use this free tool to find treatment centers in your area.
Frequently Asked Questions About Addiction
We’ve compiled some of the most frequently asked questions about addiction and its treatment.
What is at the root of addiction?
Addiction isn’t a simple issue. Often, people who develop an addiction struggle with overlapping problems involving genetics, environment, and more. There isn’t a single cause of addiction.
What is the true meaning of addiction?
Addiction is typically defined as a chronic condition that touches almost every part of a person’s life.
What percentage of addiction is genetic?
Researchers say between 40% and 60% of a person’s addiction risk is caused by genes. Other factors come into play as well, and there isn’t a sole cause of addiction.
Are there specific genes that can make you an addict?
No. Genes can increase your risk of developing an addiction. But researchers haven’t identified a specific gene that causes an addiction in everyone who has it.
What does it mean to have an addictive personality?
Bloggers and magazine writers use this term to describe people who have several addiction risk factors. If you know you have certain risk factors for addiction, you can take extra measures to prevent substance abuse in your life.
Is addiction a disease?
No. Experts consider addiction to be a disorder or chronic condition. They generally reserve the word disease for other illnesses. That being said, some addiction treatment experts still refer to addiction as a disease.
What is the most addictive drug?
The most addictive drug for one person may have no impact on another. Addictions are always personal. Some drugs do have high addiction potential, such as opioids, benzodiazepines, and alcohol.
- Definition of Addiction. (September 2019). American Society of Addiction Medicine.
- Addiction and Substance Misuse Reports and Publications. (March 2023). U.S. Department of Health and Human Services.
- 21 Million Americans Suffer from Addiction. Just 3,000 Physicians Are Specially Trained to Treat Them. (December 2019). American Society of Addiction Medicine.
- Provisional Data Shows U.S. Drug Overdose Deaths Top 100,000 in 2022. (May 2023). Centers for Disease Control and Prevention.
- Understanding the Opioid Overdose Epidemic. (June 2022). Centers for Disease Control and Prevention.
- Drug Misuse and Addiction. (June 2022). Centers for Disease Control and Prevention.
- Syndrome, Disorder, and Disease. (January 2015). Encyclopedia of Clinical Psychology.
- Addiction and Health. (July 2020). National Institute on Drug Abuse.
- Substance Use Disorders. (May 2020). National Alliance on Mental Illness.
- Alcohol-Related Emergencies and Deaths in the United States. (2023). National Institute on Alcohol Abuse and Alcoholism.
- Is Marijuana Addictive? (July 2020). National Institute on Drug Abuse.
- Alcohol Poisoning Deaths. (January 2015). Centers for Disease Control and Prevention.
- Hallucinogens. (April 2020). Drug Enforcement Administration.
- The Drug Overdose Epidemic: Behind the Numbers. (May 2023). Centers for Disease Control and Prevention.
- Drug Overdose Death Rates. (February 2023). National Institute on Drug Abuse.
- Myths About Substance Use Disorders. Indian Health Service.
- Free Will and the Brain Disease Model of Addiction: The Not So Seductive Allure of Neuroscience and Its Modest Impact on the Attribution of Free Will to People with an Addiction. (November 2017). Frontiers in Psychology.
- Addiction as a Brain Disease Revised: Why It Still Matters, and the Need for Consilience. (February 2021). Neuropsychopharmacology.
- Re-socializing the Vulnerable Brain: Building an Ethically Sustainable Brain Disease Model of Addiction. (December 2018). Frontiers in Sociology.




